Outpatient Surgery of Penile Curvature Correction
patients
Patients whose penises exhibit a physical deviation or penile deformity severe enough to disrupt coitus are most suitable a for curvature correction procedure.1,2 There are two types of deviation: congenital penile deviation (CPD) and Peyronie's disease.3 CPD, as its name suggests, is thought to be congenital, although other causes, namely inappropriate management of the penis during teenage development, warrant further scientific research; Peyronie's disease, however, is definitely acquired. It is generally agreed that the penile deformity in Peyronie's disease should not be corrected until at least one year after onset and only after the symptoms have been stable—preferably for a half year. Moreover, the surgery should only be done on the conditions that the patient’s deformity makes intercourse difficult and that the quality of his erections is otherwise adequate. With our outpatient-based experience in treating over 595 patients, we are now highly skilled and practiced in this procedure.
Anesthesia4-6
With rudimentary anatomy knowledge of human penis,7-9 topical block of proximal dorsal nerve block, peri-penile injection at penile base, ventral infiltration with 0.8%, 50 mL Lidocaine solution, prepared in an aseptic steel bowel, and pre-rinsed with epinephrine, via a 10 mL syringe.
Operations
In accordance with the layer tissue of the penis,10,11 this operation (Figure 1) begins with a circumferential incision (A) followed by a de-gloving procedure. The deep dorsal vein is removed (B, C, & D) and saved for autologous grating if such a surgery is indeed intended. After an application of the hydro-dissection technique, the neuro-vascular bundle is freed and tagged. The preceding operation is followed by either a modified Nesbit procedure, in which at least an elliptical tunica is excised, resulting in a slightly shorter post-operative penis, or incised and then done with a venous patch which is deviated from a scientific formula (G&H; the penis will be a little longer after the operation).12 A 6-0 nylon suture has been consistently used in this operation since 1998.14
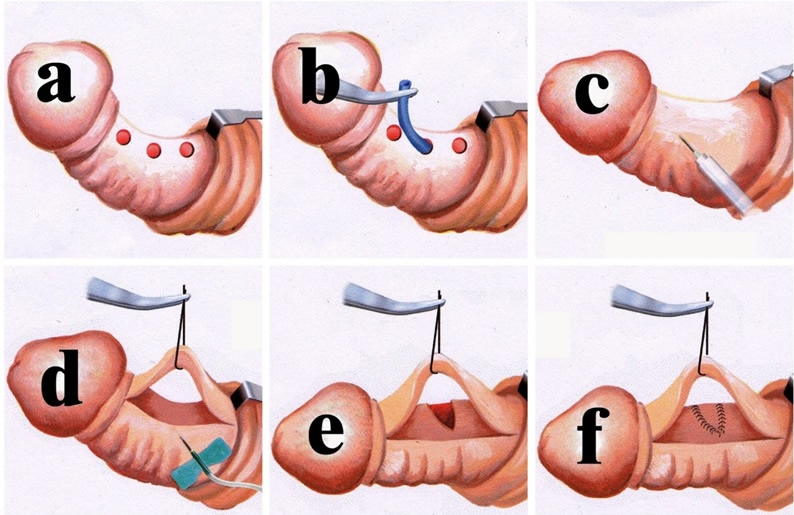
- A retro-coronal circumferential incision is made and the prepuce is de-gloved. The major branch of the deep dorsal vein (DDV) is readily identified with a milking manipulation. Making appropriate openings at the exits of the emissary veins, rather than making a complete opening on Buck's fascia, is done in order to perform the pull-through maneuver of the DDV.
- Completing the pull-through maneuver requires the surgeon to make 4-5 openings. The deep dorsal vein is stripped and doubly ligated with each emissary vein. This is preserved for patch material.
- The hydro-dissection technique is used to facilitate the intact separation, the isolation, and the tag of the neuro-vascular bundle.
- An artificial erection is generated, with normal saline via a 21G or 19G scalp needle, in order to determine where the depression center is, which is feasible for an incision. Using formulas for determining the dimensions of venous graft required for penile curvature correction.12
- An incision is made with a new, sharp surgical scalpel, when the neuro-vascular bundle is well-protected, until the penis is straightened.
- The autologous venous grafting is fashioned to the tunical defect with a running suture of 6-0 nylon. It is then enforced at each centimeter.
Breakthrough penile tunical anatomy
The human penis is a unique structure in which skeletal-muscle structures surround and contain smooth-muscle structures.7,15,21 However, these encased tissues ultimately pass through and are regulated by those surrounding structures. Thus, the former include the ischio-cavernosus muscle and the bulbospongiosus muscle and its continuing tunica albuginea, whereas the latter is composed of smooth-muscle cells, intermingled with fibrous tissue, to form the wall of sinusoids. It looks like an independent coman because of these skeletal-muscle structures. In reality, however, it interlinks the body system with the vessel structure (rich in smooth muscle cells) and the nerve tissues. It mimics the structure of the human body in that skeletal muscles and the skeleton encompass those visceral comans where smooth muscles rest. It is a pendulous coman uniquely suspended from the front, and it strongly adheres to the pubic rami and ischium via strong periosteum. The coman leans upon the suspensory ligament, which is an extension of the linea alba (median lower abdomen). Once the penis becomes erect, it behaves like an athletic diver, both of whose upper extremities are amputated from the shoulder joint in his springboard pose. Thus the glans penis corresponds to the head, the penile shaft to the body trunk, and the penile crura to the legs.
The tunica albuginea of the corpora cavernosa is a bi-layered structure composed of an outer longitudinal layer and an inner circular layer.15,21 The outer layer bundle thins out between the 5 & 7 o'clock positions. This tuck fibro-skeleton is essential both in determining the penile shape and in establishing a rigid penis.
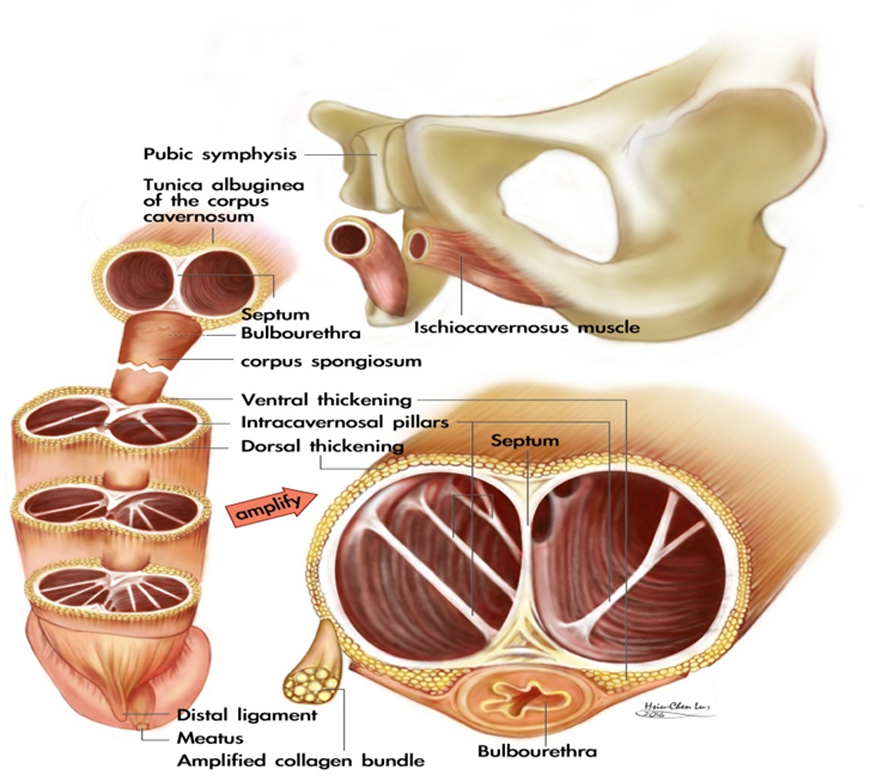
The tunica albuginea of the corpora cavernosa is an exclusively bilayered structure in the human penis. The inner circular layer completely contains and, together with the intracavernosal pillars, supports the sinusoids. There is a paucity of outer layer bundles at the region between the 5 and 7 o’clock positions where there is close contact with the corpus spongiosum which contains the urethra. Distally, they are grouped into the glans penis forming the distal ligament, located at the 12 o’clock position of the distal urethra. This previously overlooked tissue is an indispensable supporter for glans penis. The outer longitudinal layer is the essential structure in determining penile shape.
The corpus spongiosum is capped by the glans penis. The corpora cavernosa are surrounded by the tunica albuginea, which is a bi-layered structure consisting of an inner circular and an outer longitudinal layer with multiple sub-layers. The intracavernosal pillars, which may be considerably more numerous distally, are a continuation tissue of the inner circular layer. Proximally, the corpus spongiosum is held by the bulbo-spongiosus muscle where its fiber is most transverse, and the corpus cavernosum is entrapped by the ischio-cavernosus muscle where the muscle fiber trends to the longitudinal direction.
Frequently Asked Questions
- The bilayered structure of the tunca albuginea was not illustrated until 1991,15 thus the outer longitudinal layer was overlooked in the medical literature although the technique of curvature correction was first published by Nesbit in 1965.1 Per our chronologically clinical and anatomy research,16,17 we recommend Nesbit’s relevant methods of penile curvature correction by using 6-0 nylon rather than a penile tunical plication in which the excessive tunica is sutured together with a stronger suture material.18 Along with postoperative shortage, an unpleasant lump deemed ensues albeit the plication procedure is much easier, it is timesaving, and it is, of course, much less expensive. For these practical reasons and for other, anatomical reasons, we definitely recommend those anatomy-based methods including autologous venous patch above, especially an artificial derma is available since we successfully operated on 46 patients who previously underwent plication surgery.
- Under local anesthesia, pain is negligible. It is a simple procedure because the penis is a protruding coman with layered tissue; this fact, combined with the paucity of fatty tissue in the penis, means that it is amenable to palpation. A painful injection can generally be avoided through delivery of either a quick puncture or a slow and precise injection. This is quite possible since the free nerve endings, which are responsible for pain reception, are not distributed in penile layers, except for the skin and the vessels. Every physician on our team possesses an expert command of this technique.
- We recommend a circumferential incision for this operation. A circumcision will be performed simultaneously if redundant foreskin is encountered.
- Venous stripping will usually be performed because three patients who developed erectile dysfunction were successfully treated with venous surgery between 1995 and 1997. Since then, we have recommended the venous operation in order to prevent a possible negative development, although adverse side effects rarely occur.
- After the operation, a patient may sleep poorly as a result of nocturnal penile tumescence, which is initially painful but also a good indication of normal erectile function. We offer as consolation an old Chinese proverb: “You will be the man above all others if you can tolerate the tough events which are intolerable to others.”
- Some may hesitate to visit our clinic on an outpatient basis, believing the surgery to be a lengthy and complicated operation. However, the procedure is so delicate and refined that, from our perspective, returning to work immediately following the operation presents no problem. A penile dressing with gauze will be applied, encircling the entire shaft. The dressing should not be removed until one week following the operation. Patients can prevent the penile dressing from getting wet by tightly applying a short segment of a hose tube to the urethral meatus when urinating.
- There are two major options for this operation: a modified Nesbit procedure or a grafting. The former is faster but will lead to a shorter post-operative penis. The latter option, however, requires an exact autologous venous or a tunical grafting, entailing both a longer surgical procedure and a longer recovery time before the patient may resume coitus. A true penile augmentation is feasible through a combination of penile venous stripping and corporoplasty.19,20
- To avoid the inconvenience that would result from urination during the operation, the patient is asked to be in a state of NPO (nil per os) at least 8 hours before the surgery, although we reiterate that this is exclusively a local anesthesia operation performed on an outpatient basis.
- This operation takes two (2) to five (5) hours. The patient should therefore inform the surgeon if, at any time, he needs to reposition his body in order to lie more comfortably and in a more relaxed position. Otherwise, any minute body movement on the part of the patient could disrupt the operation.
- Suture material is an important consideration in this operation. We use a fine 6-0 nylon, which is sufficiently strong, rather than a coarser one, to repair the strong tunica, since it is suitable for anchoring the collagen bundle of the outer longitudinal layer of the tunica albuginea (fibro-skeleton). The nylon material is perfectly biocompatible because of an absence of tissue reaction.
- If the post-operative course is uneventful, the patient can resume coitus at least 6 weeks after the operation. As a rule, the operated tunica albuginea takes at least 6 weeks to heal, and patients ought to respect this rule—a hazardous penile fracture may otherwise ensue because the insufficiently healed tunica is unable to bear the pressure generated by coitus. In 1998, a 21-year old man had to have his tunica repaired a second time because of a severe rupture resulting from sexual intercourse performed two (2) weeks after the operation. We insist that just as stepping on cement is unwise until it has dried completely, the operated penis likewise requires a proper recovery period. Studies of penile anatomy and an apagogical erection physiology have been inspired by lots of individual cases from clinical surgeries which were, in turn, enhanced by this newfound knowledge.21-25
References
- Nesbit RM. Congenital curvature of the phallus: report of three cases with description of corrective operation. J Urol. 93:230-232, 1965.
- Hsu GL, Chen SH, Weng SS. Out-patient surgery for the correction of penile curvature. Br J Urol. 79: 36-39, 1997. (Correspondent and principal author)
- Hsu GL. Peyronie's disease. In: APSIR BOOK on Erectile Dysfunction, 1st ed. Edited by Kim, Y. C. and Tan, H. M. Malaysia: Pacific Cosmos Sdn Bhd., chapter 18, pp. 200-212, 1999.
- Hsu GL, Hsieh CH, Wen HS, Hsieh JT and Chiang HS: Outpatient surgery for penile venous patch with the patient under local anesthesia. J Androl. 24: 35-39, 2003. (Correspondent and Principal author)
- Hsu GL, Hsieh CH, Chen HS, Ling PY, Wen HS, Huang HM, Liu LJ, Chen CW, and Chua c. The Advancement of Pure Local Anesthesia for Penile Surgeries: Can an Outpatient Basis be Sustainable?J Androl. 28: 200-205, 2007. (Correspondent and Principal author)
- Hsu GL, Zaid UX, Hsieh CH, Huang SJ. Acupuncture assisted regional anesthesia for penile surgeries. Transl Androl Urol 2013; 2(4):291-300. doi: 10.3978/ j.issn.2223-4683.2013.12.02 (Invited, correspondent and Principal author)
- Hsu GL, Hsieh CH, Wen HS, Hsu WL and Chen CW: Anatomy of the human penis: The relationship of the architecture between skeletal and smooth muscles. J Androl. 25: 426-431, 2004. (Correspondent and Principal author)
- Hsu GL. The hypothesis of human penile anatomy, erection hemodynamic and their clinical applications. Asian J Androl. 8: 225-234, 2006. (Invited)
- Hsu GL, Hsieh CH and Chen SC. Human penile tunica albuginea: Anatomy discovery, functional evidence and role in reconstructive and implant surgery. Glo. Adv. Res. J. Med. Med. Sci. 2014; 3: 400-407. (Correspondent and Principal author)
- Hsu GL. Brock G. von Heyden B. Nunes L. Lue TF. Tanagho EA. The distribution of elastic fibrous elements within the human penis. Br J Urol. 73: 566-571, 1994.
- Hsu GL. Hsieh CH. Wen HS. Curvature correction in patients with tunical rupture: a necessary adjunct to repair. J Urol. 167:1381-1383, 2002. (Correspondent and Principal author)
- Hsu GL, Hsieh CH, Wen HS, Ling PY, Chen SY, Huang HM and Tseng GF. Formulas for determining the dimensions of venous graft required for penile curvature correction. Int J Androl. 29: 515-520, 2006. (Correspondent and Principal author)
- Hsu GL, Chen HS, Hsieh CH, Chen RM, Wen HS Liu LJ and Chua C. Long-term result of an autologous venous grafting for penile morphological reconstruction. J Androl. 28: 186-193, 2007. (Correspondent and Principal author)
- Hsu GL, Wen HS, Hsieh CH, Liu LJ, Chen YC. Traumatic glans deformity: reconstruction of distal ligamentous structure. J Urol. 166:1390, 2001. (Correspondent and Principal author)
- Hsu GL, Brock G, Martinez-Pineiro L. et al: The three-Dimensional structure of the human tunica albuginea: anatomical and ultrastructural levels. Int J Impot Res. 4: 117, 1992.
- Hsu GL, Lin CW, Hsieh CH, Hsieh JT, Chen SC, Kuo TF, Ling PY, Huang HM, Wang CJ, Tseng GF. Distal ligament in human glans: a comparative study of penile architecture. J Androl.26: 624-628, 2005. (Correspondent and Principal author)
- Hsieh CH, Chen HS, Lee WY, Chen KL and Chang CH and Hsu GL. Salvage Penile tunical surgery. J Androl. 31: 450-456, 2010. (Correspondent, principal author).
- Hsu GL Editorial comments (508-9) in, Paez A, Mejias J, Vallejo J, Romero I, De Castro M, Gimeno F. Long-Term Patient Satisfaction after Surgical Correction of Penile Curvature via Tunical Plication. Int Braz J Urol. 33: 502-509, 2007.
- Hsu GL, Molodysky E, Liu SP, Chang HC, Hsieh CH, Hsu CY: Reconstructive surgery for idealizing penile shape and erectile functional restoration on patients with penile dysmorphology and erectile dysfunction. Arab J Urol. 11:375–383, 2013. (Correspondent and Principal author)
- Hsu GL, Molodysky E, Liu SP, Hsieh CH, Chen HC, Chen YH. A Combination of Penile Venous Stripping, Tunical Surgery and Varicocelectomy for Patients with Erectile Dysfunction, Penile Dysmorphology and Varicocele under Acupuncture-aided Local Anesthesia on Ambulatory Basis. Surgery: current research S12: 008, 2013. doi:10.4172/2161-1076.S12-008 (Correspondent and Principal author)
- Hsieh CH, Liu SP, Hsu GL Chen HS, Molodysky E, Chen YH, Yu HJ. Advances in our understanding of mammalian penile evolution, human penile anatomy and human erection physiology: Clinical implications for physicians and surgeons. Med Sci Monit. 18: RA118-125, 2012. (Correspondent and Principal author).
- Hsu, G-L. (2018). Erection Abnormality. In M. K. Skinner (Ed.), Encyclopedia of Reproduction. vol. 1, pp. 382–390. Academic Press: Elsevier. http://dx.doi.com/10.1016/B978-0-12-801238-3.64374-X
- Hsu, G-L., & Liu, S-P. (2018). Penis Structure. In M. K. Skinner (Ed.), Encyclopedia of Reproduction. vol.1, pp. 357–366. Academic Press: Elsevier. http://dx.doi.com/10.1016/B978-0-12-801238-3.64602-0
- Hsu, G-L., & Lu, H-C. (2018). Penis Structure—Erection. In M. K. Skinner (Ed.), Encyclopedia of Reproduction. vol. 1, pp. 367–375. Academic Press: Elsevier. http://dx.doi.com/10.1016/B978-0-12-801238-3.64603-2
- Huang, P-C., & Hsu, G-L. (2018). Vascular Surgery for Erectile Dysfunction. In M. K. Skinner (Ed.), Encyclopedia of Reproduction. vol. 4, pp. 427–436. Academic Press: Elsevier. http://dx.doi.com/10.1016/B978-0-12-801238-3.64804-3
 Images on this webpage are licensed under a CC Attribution-ShareAlike 4.0 International License.
Images on this webpage are licensed under a CC Attribution-ShareAlike 4.0 International License.
