Penile Enhancement in Implant Patient
patients
Although penile implant remains a final solution for patients with refractory impotence,1,2 undesirable post-operative effects in particular the size reduction and the cold sensation of the glans penis remain problematic.3,4 Herein we have developed a novel method of glandular enhancement resulting from venous ligation of the retrocoronal plexus and proximal channels of the deep dorsal and cavernosal veins on ambulatory basis since 2003.5-10 This surgery can be a viable option although some dissatisfied implant patients may be with certain, primarily either cosmetic or subjectively unhappy outcomes of prior operation, such as postoperative penile length or a cold, small glans penis.
Anesthesia
Same as the session of E, but the needle for the injection of local anesthetic is not allowed to penetrate through the tunica albuginea.
Operation
The surgery begins with a semi-circumcision where the retrocoronal plexus is ligated one-by-one with a 6-0 nylon suture. Then the medial longitudinal incision is made in order to perform the first 90-degree Z-plasty, which is made in the pubic region and used for advancement of penopubic skin, which then becomes the skin of the penile base. The suspensory ligament is severed and the collagen bundles are detached from the arcuate ligament and released as much as possible; meanwhile, the deep dorsal vein, cavernosal vein and the para-arterial vein are likewise ligated. The skin is repaired with a 6-0 nylon or 5-0 chromic suture. The second 90-degree Z-plasty is made at the penoscrotal junction to elongate the penile shaft.
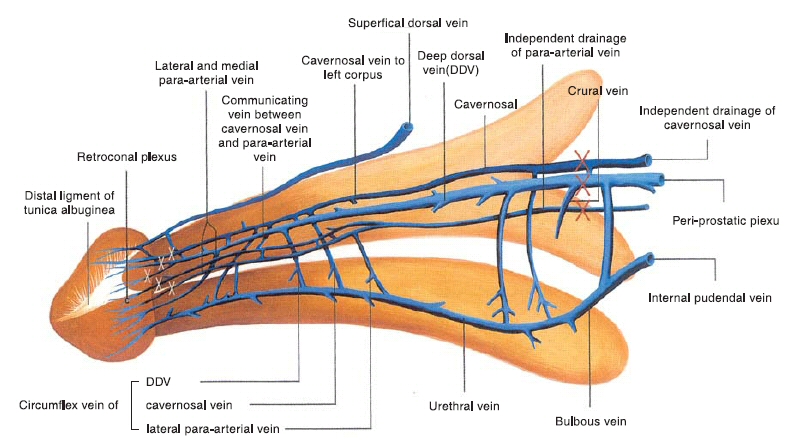
The deep dorsal vein, consistently in the median position, receives blood of emissary veins from the corpora cavernosa and of circumflex veins from the corpus spongiosum. It is sandwiched by cavernosal veins, although these lie in a deeper position. Bilaterally, the dorsal arteries are sandwiched by a medial and a lateral para-arterial vein respectively. They are ligated at the level of the penile hilum. Likewise the veinlets of the retrocoronal plexus are ligated with a 6-0 nylon suture.
Two representative cases are demonstrated via cavernosography.9 The augmentation of the glans penis can be demonstrated by some increment of glans radius (Figure 2) and particularly penile shaft length (Figure 3) if patient request.
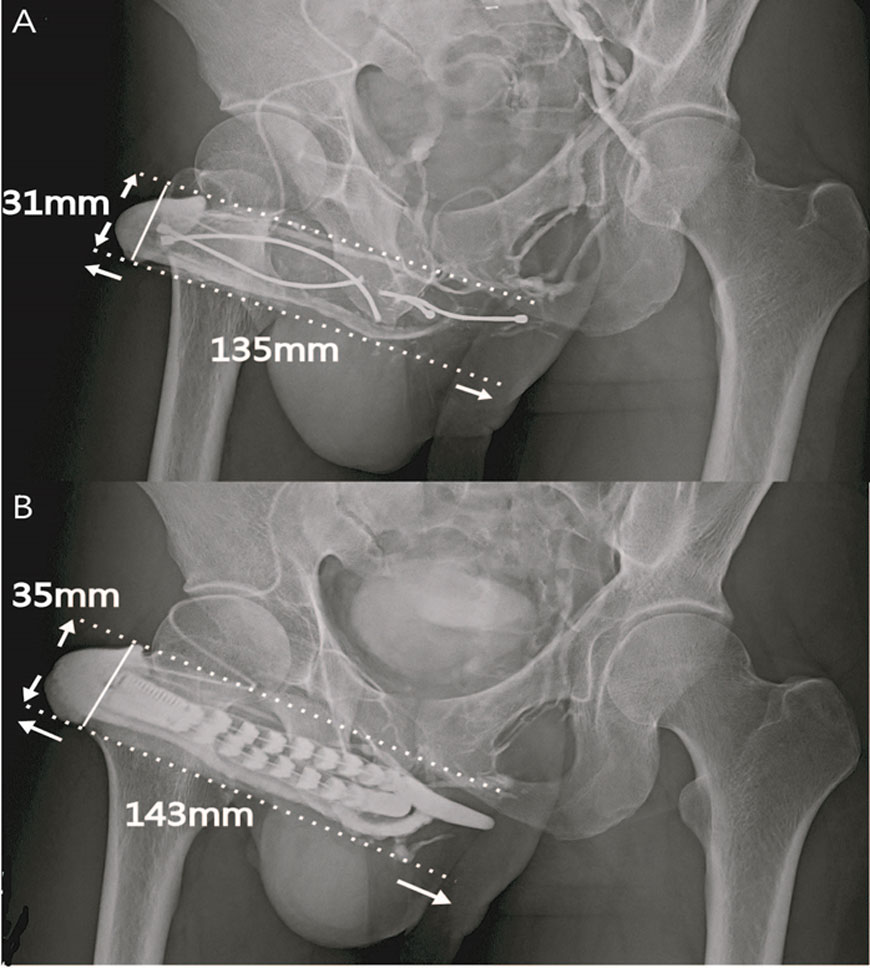
He underwent the first surgery of penile implant with AMS600 in 2004. A mechanical failure of penile prosthesis prompted him to receive a Spectra implant revision, and he chose to commit to the additional venous ligation surgery. A. The glanular radius was enhanced from 31mm to 35mm after the penile venous surgery. B. The DDV and CVs were ligated at the level of the retrocoronal and hilum regions respectively. Enhancement was shown both in the glans penis and the entire penile shaft after a contract medium was injected to the glans penis via a #23 scalp needle.
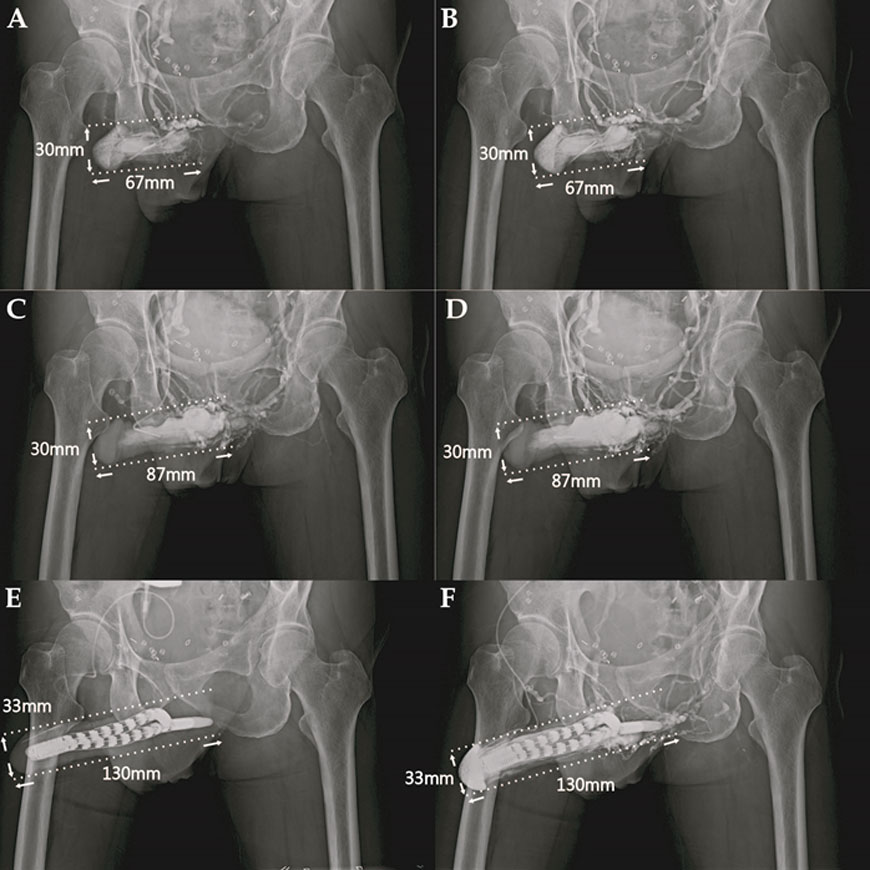
He underwent cryosurgery for prostate adenocarcinoma elewhere in 2010. ED and ventral penile deformity prompted him to underwent Spectra implantation.
- Cavernosogram was made after 20ml of contract medium was injected. The glandular radius and penile length was 30mm and 67mm respectively.
- Cavernosogram was undertaken after another 30ml of contract medium was injected. Note the penile dimension remained the same.
- The penile tissue sustained limited extension 30 min after 20 μg prostaglandin E1 (PGE1) was injected intracavernously. The penile length could merely reach to 87mm. The venous leakage was proved because the drainage veins are conspicuous despite an intracavernosal pressure exceeded 110mmHg.
- Both penile length and glanular radius remained the same despite another 30 ml solution was infused.
- The venous surgery was performed for penile enhancement in addition to a penile implant with Spectra. The penile dimension was enhanced to 130mm penile length and 35mm glanular radius. Note that a #23 scalp needle was set in the glans penis.
- The glans was enlarged and opacified after the contrast medium was injected and drained along the corpus spongiosum. Note that the DDV and CVs were ligated around the penile.
Discussion
- After this procedure, the circulation of the penis is altered in such a way that the sinusoidal blood of the glans is drained exclusively through the corpus spongiosum via the bulbourethral vein. This can explain why the glans penis gradually becomes enlarged after operation since an enclosed milieu is consequently established for Pascal’s principle.11 Unsurprisingly, the patient will no longer be troubled by a “cold” sensation of the glans.
- In penile implantation it is standard for the surgeon to dilate the corpus cavernosum as much as possible to house an implant of maximal size. In contrast we recommend the smallest implant in order to prevent the possibility of the cavernosal artery from being compressed, which would compromise coital tumescence of the sinusoid postoperatively.
- According to our study, the drainage veinlets at the level of the retrocoronal sulcus may number as many as 29. Ligating these will confine the glanular drainage pathway to the corpus spongiosum. Meanwhile, with the deep dorsal vein, cavernosal and para-arterial vein ligated at the level of the penile hilum, the circulation of the corpora cavernosa is switched to the corpus spongiosum and to a lesser extent the superficial dorsal vein. Thus, blood flow, enhanced during coitus, is forced into the corpulatory segment of the penis. This may be responsible for the enhancement phenomenon in implant patients.
- We apply two 90-degree Z-plasties, which differ from the regular 75-degree Z-plasty. Some may question whether a Z-plasty can be extended to 90 degrees. As far as we know, the extensibility of the exogenitalia area is overwhelming; therefore, the design of 90 degrees is feasible.
References
- Montague DK. Experience with semirigid rod and inflatable penile prosthesis. J Urol 1983; 129: 967-968.
- Kaufman JJ, Lindner A, Raz S. Complications of penile prosthesis surgery for impotence. J Urol 1982; 128: 1192-1194.
- Wilson SK, Delk JR, Salem EA, et al. Long-term survival of inflatable penile prostheses: single surgical group experience with 2384 first-time implants spanning two decades spanning two decades. J Sex Med 2007; 4: 1074–1079.
- Montorsi F, Guazzoni G, Bergamaschi F et al. Patient-partner satisfaction with semirigid penile prostheses for Peyronie's disease: a 5-year followup study. J Urol, 1993; 150: 1819-1821.
- Hsu GL, Brock G, Martinez-Pineiro L et al. The three-dimensional structure of the tunica albuginea: anatomical and ultrastructural levels. Int J Impot Res 1992; 4: 117-,
- Hsu GL. Hsieh CH. Wen HS, Chen SC, Chen YC, Liu LJ, Mok MS and Wu CH. Outpatient penile implantation with the patient under a novel method of crural block. Int J Androl. 2004; 27: 147-151. (Correspondent and Principal author)
- Hsu GL, Chen HS, Huang SJ. Does tunica anatomy matter in penile implant? Transl Androl Urol 2014; 4(4):406-412. doi: .3978/j.issn.2223-4683.2014.03.04 (Correspondent and Principal author)
- Hsu GL, Hsieh CH, Wen HS et al. Penile enhancement: an outpatient technique. Eur J Med Sexology 2002; 11: 7.
- Hsu GL, Hill JW, Hsieh CH, Liu SP and Hsu CY: Venous ligation: A novel strategy for glans enhancement in penile prosthesis implantation. BioMed Res Int Volume 2014 Article ID 923171, 7 pages, 2014. http://dx.doi.com/10.1155/2014/923171 (Principal author)
- Breza J, Aboseif SR, Orvis BR et al. Detailed anatomy of penile neurovascular structures: surgical significance. J Urol 1989; 141: 437-443.
- Hsu GL. The hypothesis of human penile anatomy, erection hemodynamic and their clinical applications. Asian J Androl. 2006;8: 225-234. (Invited)
- Hsu GL, Hill JW, Hsieh CH, Liu SP and Hsu CY: Venous ligation: A novel strategy for glans enhancement in penile prosthesis implantation. BioMed Research International Volume 2014 Article ID 923171, 7 pages, 2014. http://dx.doi.com/10.1155/2014/923171 (Principal author)
- Hsu, G-L. (2018). Erection Abnormality. In M. K. Skinner (Ed.), Encyclopedia of Reproduction. vol. 1, pp. 382–390. Academic Press: Elsevier. http://dx.doi.com/10.1016/B978-0-12-801238-3.64374-X
- Hsu, G-L., & Liu, S-P. (2018). Penis Structure. In M. K. Skinner (Ed.), Encyclopedia of Reproduction. vol. 1, pp. 357–366. Academic Press: Elsevier. http://dx.doi.com/10.1016/B978-0-12-801238-3.64602-0
- Hsu, G-L., & Lu, H-C. (2018). Penis Structure—Erection. In M. K. Skinner (Ed.), Encyclopedia of Reproduction. vol. 1, pp. 367–375. Academic Press: Elsevier. http://dx.doi.com/10.1016/B978-0-12-801238-3.64603-2
- Huang, P-C., & Hsu, G-L. (2018). Vascular Surgery for Erectile Dysfunction. In M. K. Skinner (Ed.), Encyclopedia of Reproduction. vol. 4, pp. 427–436. Academic Press: Elsevier. http://dx.doi.com/10.1016/B978-0-12-801238-3.64804-3
 Images on this webpage are licensed under a CC Attribution-ShareAlike 4.0 International License.
Images on this webpage are licensed under a CC Attribution-ShareAlike 4.0 International License.
