Ambulatory Surgery of a Novel Factual Penile Enhancement
Introduction and Objective
Breaking news: After decades of surveillance, innovative erection restoration and corporeal augmentation ensure, which benefits the patient.
Both conventional penile venous surgery for erection restoration and surgery for penile augmentation have been controversial. Based on De Novo penile fibrovascular assembly, an innovative penile venous stripping surgery (PVSS) and factual penile girth enhancement (FPGE) ensues.
Methods and Procedure
From 2013 to 2023, refractory impotence and dysmorphia prompted 31 patients to seek PVSS and FPGE.
The Surgical Technique
PVSS (Penile Venous Stripping Surgery): This involves stripping erection-related veins, primarily one deep dorsal vein and a pair of cavernosal veins, after ligating each emissary vein closest to the outer tunica albuginea using 6-0 nylon.
FPGE (Factual Penile Girth Enhancement): This is performed along the tunica albuginea bilaterally; then, the two tunic defects were fashioned with a 70.0x30.0 mm venous stripe and covered with autologous venous walls. The penile girth was measured, and radio-opaque contrast was used to compare intracorporeal retention.

A) First circumferential incision. B) Second circumferential incision and detubularization. C) Preputial flap. D) Fashioning of flap. E) First Z-plasty on pubic region. F-H) Secondary Z-plasty on penoscrotal region.
Anesthesia Protocol
Acupuncture-assisted local anesthesia has been applied since 1988. Lidocaine solution (0.8%, 50 ml) is prepared in an aseptic steel bowl prerinsed with epinephrine. A 23-G needle with the bevel parallel to the longitudinal body axis is inserted into the periosteum along the pubic angle. The solution is injected via a 10-ml syringe in three directions: the penile hilum and the proximal dorsal nerve bilaterally.
The anesthetic effect can be confirmed by pinching the glans and local skin with toothed forceps. The dosage of lidocaine should not exceed 400 mg, through which an ambulatory basis is unexceptional.
Clinical Results
The follow-up period was 5.3±1.6 years. In the surgery group, the radiopacity of the postoperative radiopacity was consistently enhanced.
- Function Improvement: There was a significant improvement (both P< 0.01) in IIEF-5 and EHS scores (9.7±2.8 vs. 20.8±2.3; 1.7±0.6 vs. 3.2±0.2, respectively).
- Size Increase: Both the diameters of the glans and penile shaft increased (28.0±2.3mm and 28.3±2.1mm vs. 35.3±2.2mm and 36.3±2.1mm respectively).
- Satisfaction: The satisfaction rate was 81.3% (13/16) by patients. Notably, patients’ self-esteem soared as the glans penis was added physiologically, adding at least 25%.

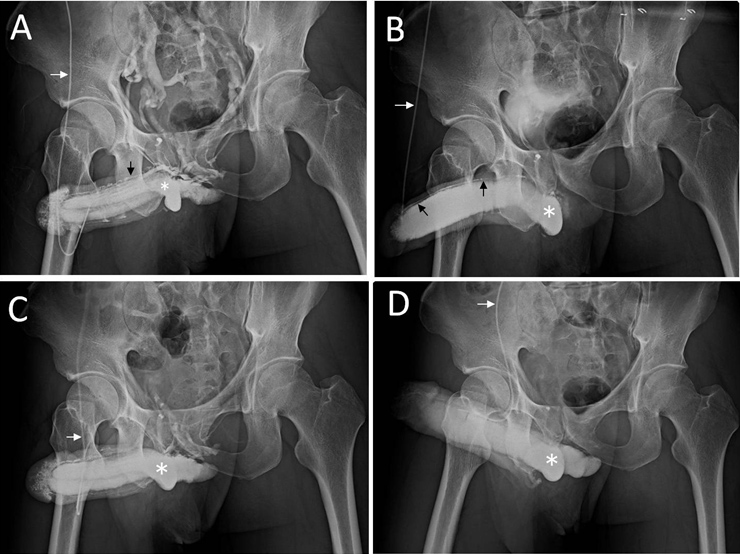
A) Pre-operative cavernosogram showing leaky veins. B) Pharmacocavernosogram demonstrating veno-occlusive dysfunction.
C) Post-operative film showing noticeable improvement in fluid retention. D) Post-operative film showing no more leaky veins and favorable penile morphology.
Discussion: Factual vs. Camouflage Enhancement
Conventionally, penile augmentation surgery is controversial both in its subjective responsiveness and postoperative results. We term the traditional strategies as "camouflage penile enhancement methods", including our earlier method using autologous prepuce.
However, we advise emergent combining PVSS and FPGE, the real augmentation of corpora cavernosa, instead of combining PVSS and camouflage penile enhancement. We have been consulted by many international males who underwent artificial acellular derma insertion elsewhere, which caused an awesome scenario in radiographic imaging at the expense of compromising the erection quality (Figure 3).
Conclusion
This novel combination of PVSS and FPGE is promising, although it is limited by its retrospective design and smaller sample size. Further validation requires a larger sample. We continue this emergent reconstructive strategy to improve patient satisfaction, which is an exclusive physiology surgery thus far.
Suggested Readings & References
- Hsu, G. L., Chang, H. C., Molodysky, E., Hsu, C. Y., Tsai, M. H., Yin, J. H., & Chen, M. T. (2025). A detailed analysis of the penile fibro-vascular assembly. J. Sex. Med, 22 (2), 225–234.
- Chung, C. H., Chang, K. S., Chen, H. S., Hsieh, Y. Y., Chang, Y. H., Hsu, G. L., Tsai, M. H., & Chueh, J. S. (2025). Combining Erection Restoration and Factual Penile Enhancement Based on Revolutionary Penile Fibro-Vascular Assembly. Archivos Españoles de Urología. 2025, 78(7): 849-858.
- Chen, H. S., Fang, C. W., Tsai, R. W. M., Hsu, C. Y., Hsu, G. L., Lu, H. C., Tsai, M. H., & Chueh, J. S. C. (2025). The Human Penile Fibro-Vascular Assembly Requires the Integrity of Ten Fibro-Ligaments. Life (Basel, Switzerland), 15 (9), 1492.
- Chung, C. H., Chen, H. S., Hsieh, Y. Y., Hsu, G. L., Hsieh, C. H., Lin, T. C., & Chueh, J. S. (2025). Strategy for Salvaging the Shrinking, Soft Glans Penis and Impending Prosthesis Loss in Patients with Penile Implants: Case Report. Archivos espanoles de urologia, 78 (8), 1116–1121.
- Hsu GL, Brock G, von Heyden B, Nunes L, Lue TF, Tanagho EA. The distribution of elastic fibrous elements within the human penis. Br J Urol 73(5): 566-71, 1994.
- Van Driel, M. F., Schultz, W. C., Van de Wiel, H. B. et al: Surgical lengthening of the penis. Br J Urol, 82: 81, 1998.
- Wessells, H., Lue, T. F. and McAninch, J. W.: Penile length in the flaccid and erect states: guidelines for penile augmentation. J Urol, 156: 995, 1996.
- Hsu, G. L., Hsieh, C. H., Wen, H. S. et al: Penile enhancement: an outpatient technique. Eur J Med Sexology, 11: 7, 2002.
- Kim, J. J., Kwak, T. I., Jeon, B. G. et al: Human glans penis augmentation using injectable hyaluronic acid gel. Int J Impot Res, 15:439, 2003.
- Hsu GL, Hill JW, Hsieh CH, Liu SP and Hsu CY: Venous ligation: A novel strategy for glans enhancement in penile prosthesis implantation. BioMed Res Int, Volume 2014 Article ID 923171.
- Huang, P-C., & Hsu, G-L. (2018). Vascular Surgery for Erectile Dysfunction. In M. K. Skinner (Ed.), Encyclopedia of Reproduction. vol. 4, pp. 427–436. Academic Press: Elsevier.
 Images on this webpage are licensed under a CC Attribution-ShareAlike 4.0 International License.
Images on this webpage are licensed under a CC Attribution-ShareAlike 4.0 International License.
